A small study showing that a new treatment designed by Stanford professors for severe depression has a 90% success rate was published in early April. The treatment is now being tested in a larger double-blinded study, according to the researchers.
Instead of focusing their efforts on creating a new treatment, researchers said they worked with existing technology and knowledge of the mechanisms in our brains that control depression to find a treatment that incorporated both elements.
“The idea behind this study stems from the question, what happens when you try to design a new treatment for mental health instead of discovering one,” said Brandon Bentzley, a clinical assistant professor of psychiatry and behavioral sciences. “This is the first treatment that was completely engineered based on basic neuroscience principles.”
The study used a small sample of 21 participants with severe depression who showed no response to any anti-depressant medication, talk therapy or other forms of electromagnetic stimulation.
“We wanted to recruit people with a primary diagnosis of major depressive disorder,” said Eleanor Cole, a postdoctoral research fellow in psychiatry.
After the study was concluded, 19 of the participants met depression remission criteria after taking a depression diagnostic test.
The participants chosen for the study had all been turned down by other trials because they were deemed to be untreatable. If medications do not improve a patient’s symptoms, they are considered to have treatment-resistant depression. Treatment-resistant depression can range from mild to severe.
“The more [anti-depressant] medications a person tries in sequence… the probability of the next medication to work decreases,” Bentzley said. “The patients that were enrolled in our clinical trials had a high degree of treatment-resistant depression.”
Each participant was given neuropsychological testing before and after the new treatment was administered. This particular study included patients who suffer from suicidal thoughts, which is unique, according to Bentzley.
“Nineteen of the 21 patients often had thoughts of wanting to end their life or suicidality, which is typically not allowed in a clinical trial,” Bentzley said. According to the researchers, after the treatment, all of the participants who initially reported suicidal thoughts reported no longer having those thoughts.
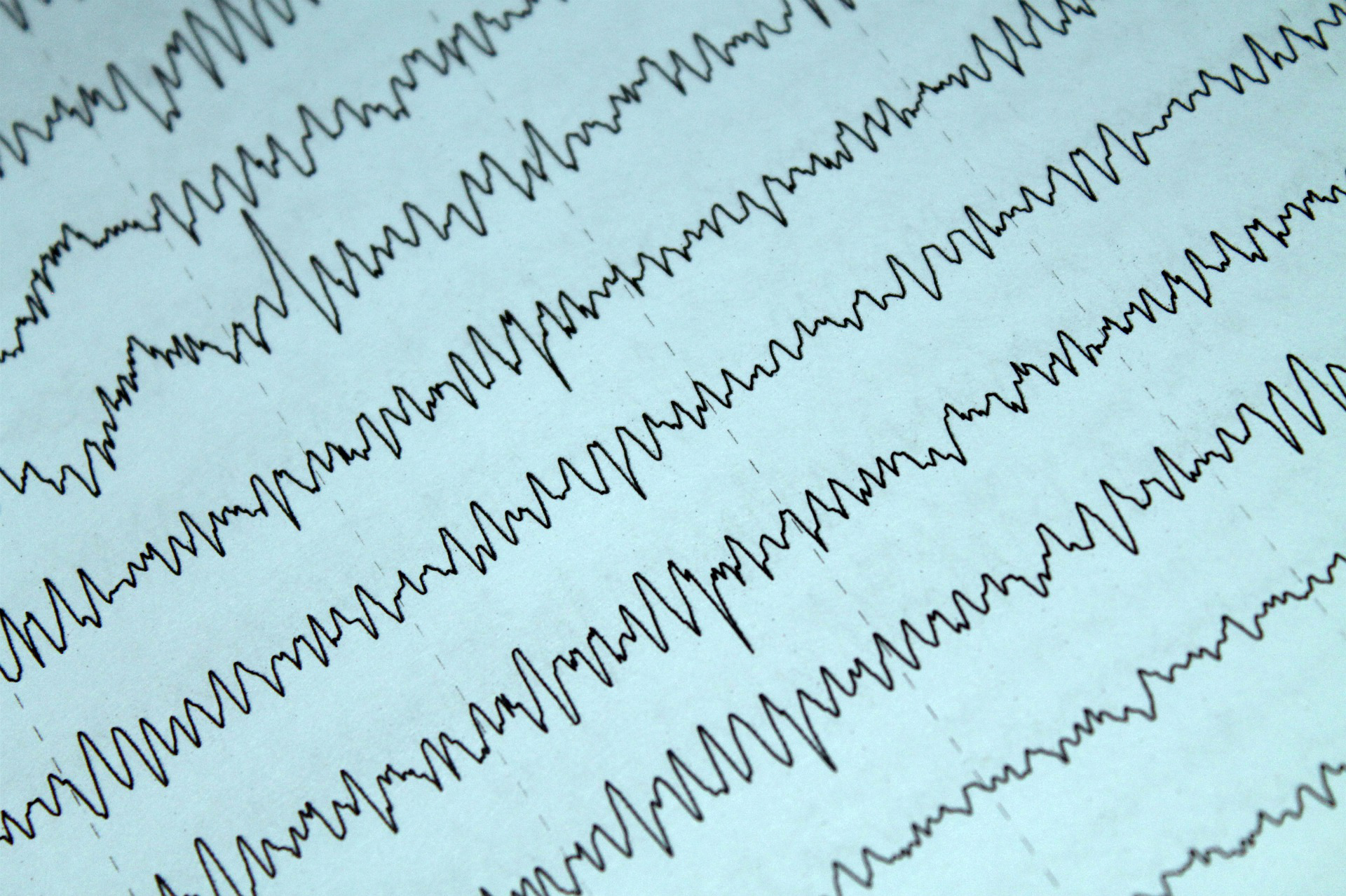
The researchers used a form of transcranial magnetic stimulation (TMS) — a non-invasive form of brain stimulation that changes magnetic fields to produce electrical currents directed to specific parts of the brain. Called Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT), it has been shown to improve current FDA-approved treatments.
One of the key differences that makes SAINT unique is the use of intermittent theta-burst stimulation (ITBS), a type of stimulation that mimics the brain’s natural firing patterns during memory processing.
Nolan Williams, associate professor of psychiatry and behavioral sciences and an author of the study, worked with his team at his lab to implement 50 therapy sessions consisting of 1,800 theta wave pulses. Traditionally, only 600 pulses are used.
The researchers are currently conducting a larger, double-blinded trial in which half of the participants will receive a fake treatment and half will receive SAINT. Participants also cannot have had the TMS treatment before, “so they can’t know what active treatment feels like,” Cole said. “During a blinded trial, that really lets us see if there is an element of a placebo effect.”
“We weren’t sure how feasible [the study] was because we were asking participants to come for multiple sessions a day… but we didn’t hear any complaints,” said Katy Stimpson, a research assistant who worked on the study. “It’s really reassuring that this is a treatment that will be very effective for the larger group.”
Contact Clyde John at cjtniles ‘at’ gmail.com.