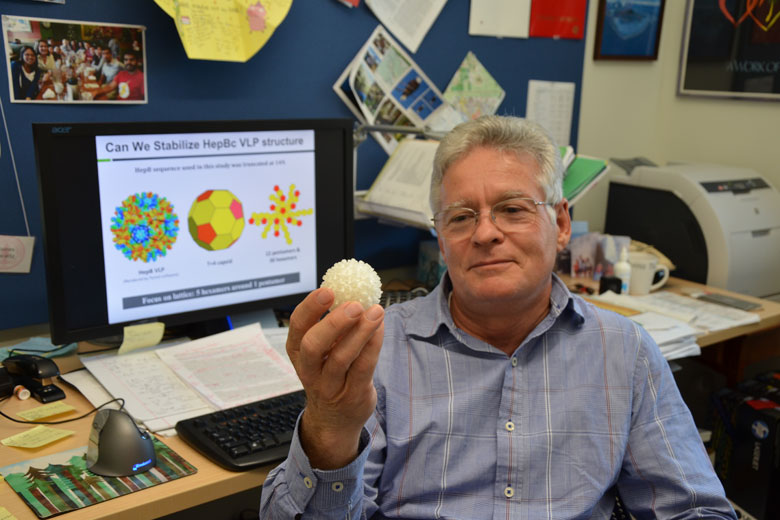
Stanford researchers have redesigned the hepatitis B virus so that it is invisible to the immune system and can target certain cells without delivering an infectious payload. This report was published in the Proceedings of the National Academy of Sciences, and professor of chemical engineering and bioengineering James Swartz, who led the report, hopes his findings will advance targeted drug delivery.
Targeted drug delivery, which enables treatment to target specific, diseased cells, is one of the main goals of modern medicine.
“We call this a smart particle,” Swartz said in a Stanford News article. “We make it smart by adding molecular tags that act like addresses to send the therapeutic payload where we want it to go.”

Viruses are similarly able to target specific cells but instead carry an infectious payload. As a result, the immune system attacks viruses in the body. Working with the virus that causes hepatitis B, Swartz and Yuan Lu, a pharmacology researcher at the University of Tokyo, took advantage of this targeting system for drug delivery.
The researchers changed the DNA of the virus – in particular, its middle layer, called the capsid – so that it appeared invisible in the immune system. This enabled the virus to travel throughout the body without being attacked. They also removed the infectious payload, opening possibilities to inject a medicinal payload instead, and changed the surface of the virus so that molecular tags can be attached to it. These molecular tags allow the virus to target only diseased cells.
Swartz explained that when he originally proposed his project, funding agencies said it couldn’t be done. After four years of work, Swartz hopes his findings will breathe new life into targeted drug delivery, where “smart particles” can deliver treatment to only harmful cells and leave healthy cells alone. This would also minimize the side effects of medication and radiation.
“This was a proof-of-principle experiment so there’s a lot of work to be done,” Swartz said. “But I believe we can use this smart particle to deliver cancer-fighting immunotherapies that will have minimal side effects.”
Swartz said the next steps are to train the immune system to recognize certain cancers by attaching cancer tags to the smart particle and then to further engineer the DNA so that protein can self-assemble around a small medicinal payload.
“That will be quite complicated, but we’ve already gotten this far when they said it couldn’t be done,” Swartz said.
Contact Jeremy Quach at jquach ‘at’ stanford.edu.